Aetna Inc
Latest Aetna Inc News and Updates
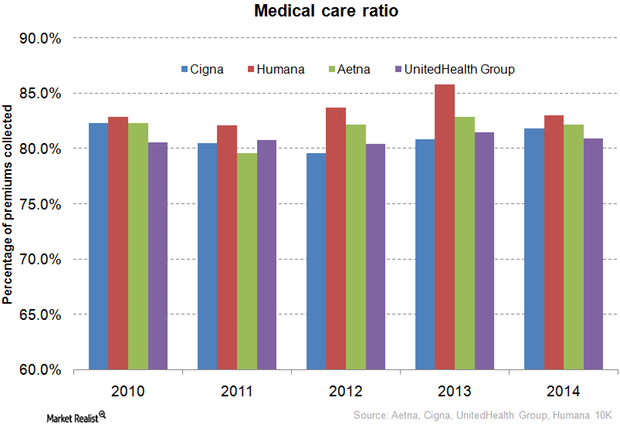
How Does Aetna Compare to Its Peers in Medical Care Ratio?
The medical care ratio of health insurance companies is calculated as the ratio of the total money spent in health care claims to premiums earned.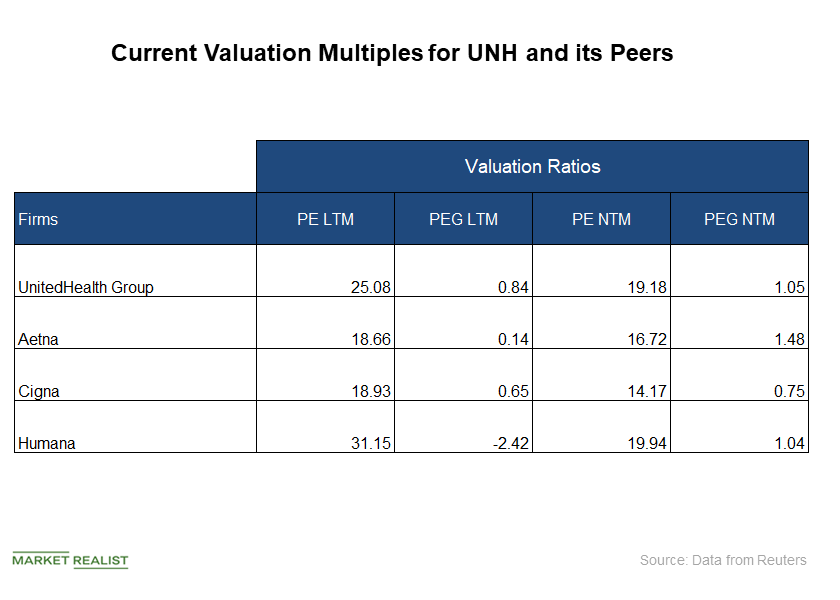
How Does UNH’s Valuation Look in October?
UnitedHealth Group is a leading managed healthcare firm in the United States.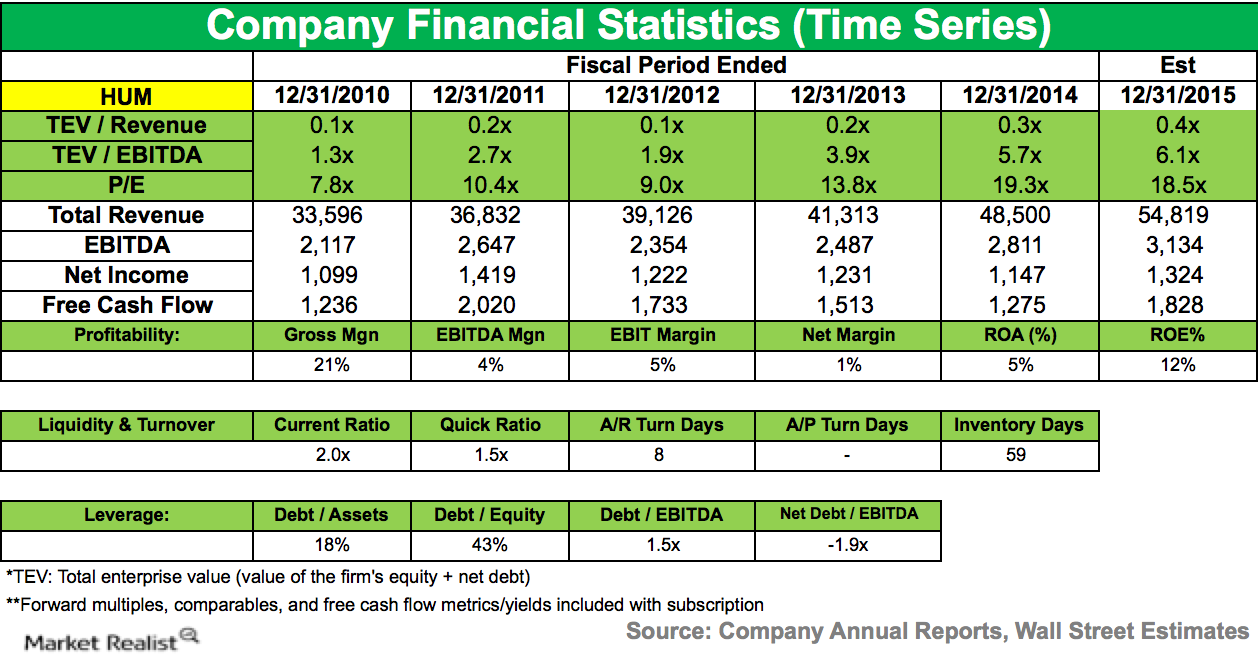
Eminence Capital Reduces Position in Humana
During the fourth quarter of 2014, Eminence Capital lowered its stake in Humana (HUM). The company accounted for 1.33% of the fund’s 4Q14 portfolio.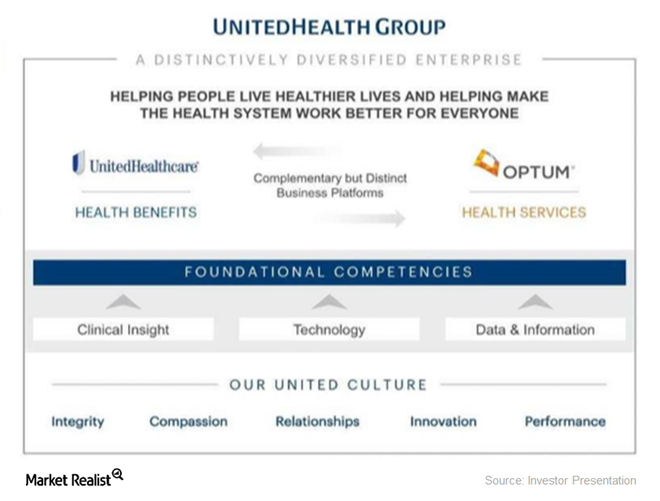
How Is UNH’s Optum Business Positioned in the Industry?
UnitedHealth Group is, by revenue, the largest healthcare company in the world.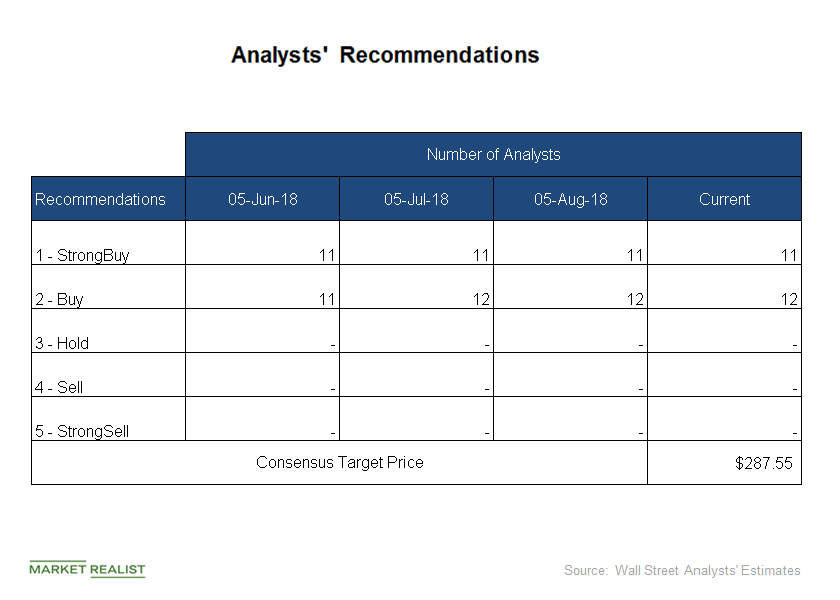
Analysts Raise Target Prices on UNH Stock in September
Of the 23 analysts covering UNH stock, all of them have “buy” or “strong buy” recommendations for UnitedHealth Group.
CVS Health versus Walgreens: Comparing Pharmacy Giants
Around 70% of the US population lives within three miles of a CVS store, while more than 75% of the population lives within five miles of a Walgreens store.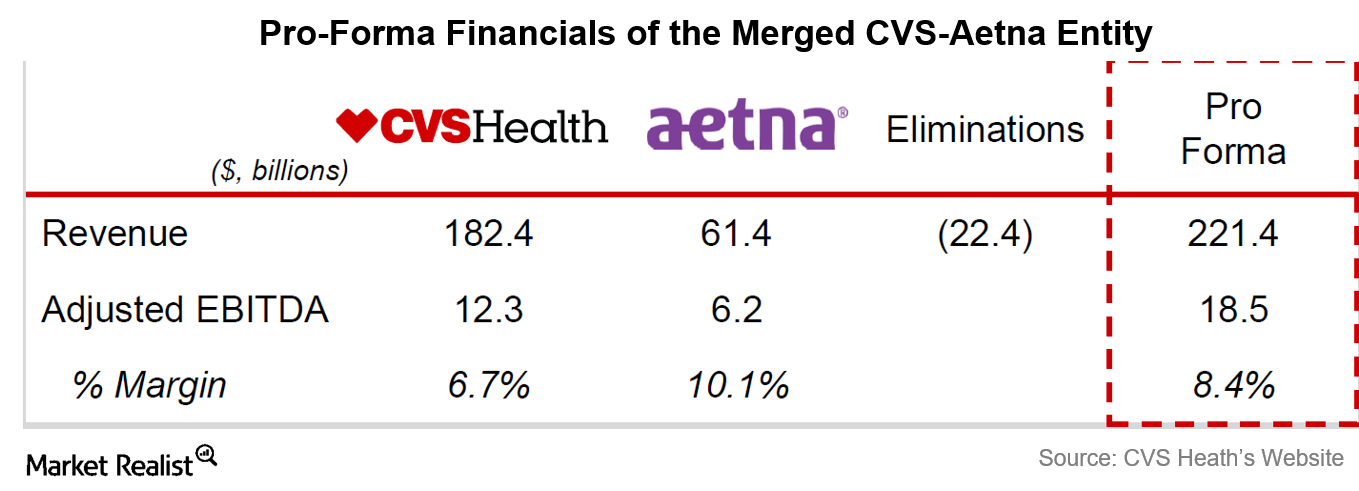
A Look at the Financial Details of the CVS-Aetna Deal
CVS is paying more than 11 times the trailing 12-month EBITDA for Aetna.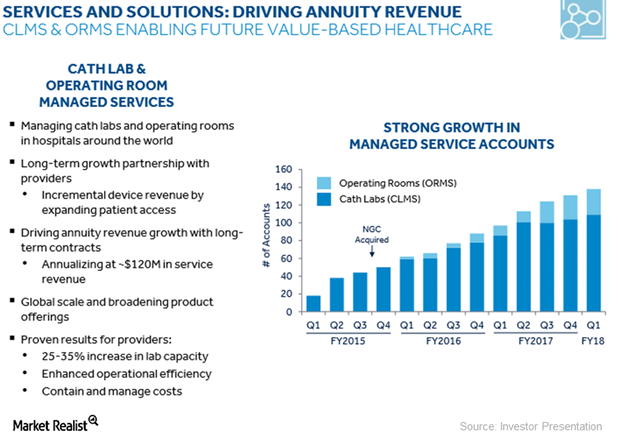
How Medtronic Is Accelerating Its Economic Value Growth Strategy
Medtronic’s (MDT) Hospital Solutions segment registered double-digit growth in fiscal 1Q18.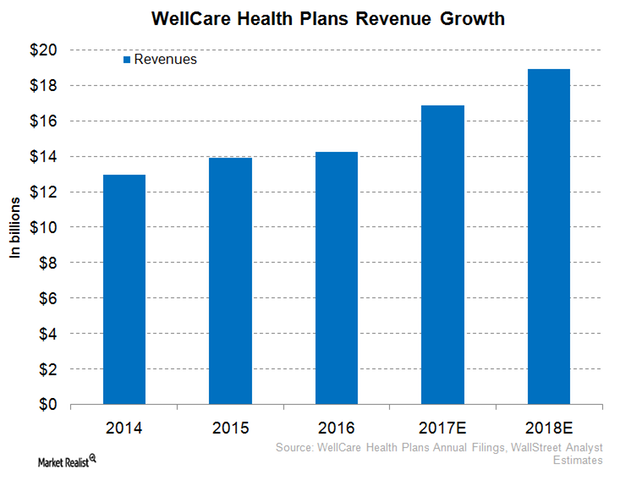
WellCare Health Plans Expects Robust Revenue Performance in 2017
In 1Q17, WellCare Health Plans (WCG) reported revenues of ~$3.9 billion, which totals year-over-year growth of around 11.7%.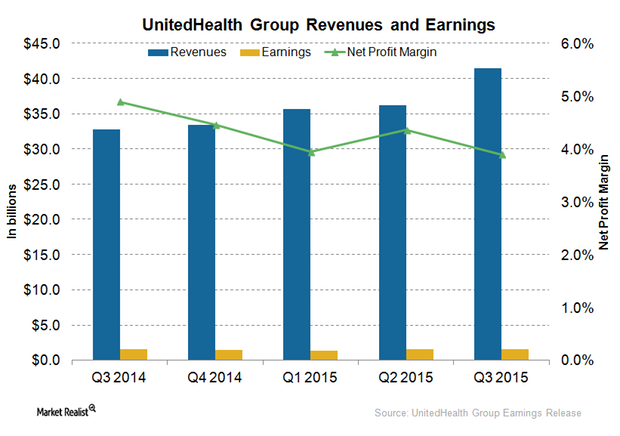
Why UnitedHealth Group’s Net Profit Margins Fell
In 3Q15, despite a rise of total revenues by 27% year-over-year, which includes 10% organic growth, UnitedHealth Group reported a decline of about 1% in net profit margins.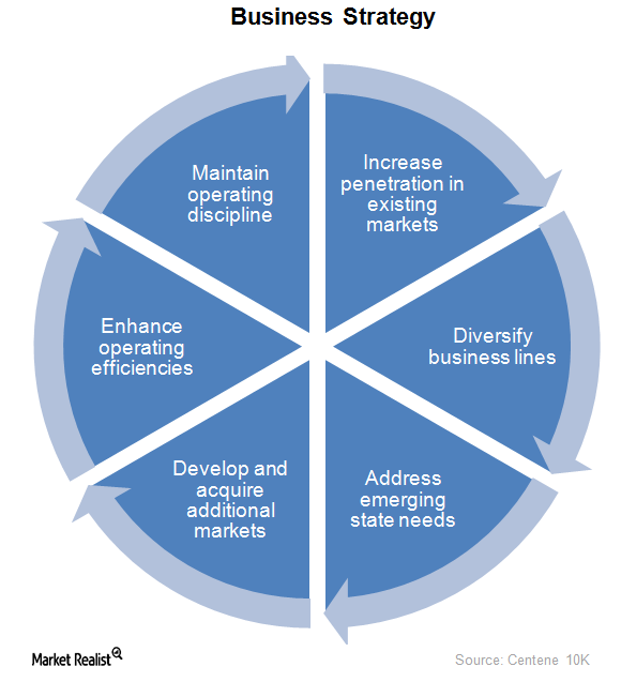
What’s Centene’s Business Strategy?
Centene’s business strategy focuses on improving the quality of its services. It provides services to the uninsured and underinsured population in 22 states in the US.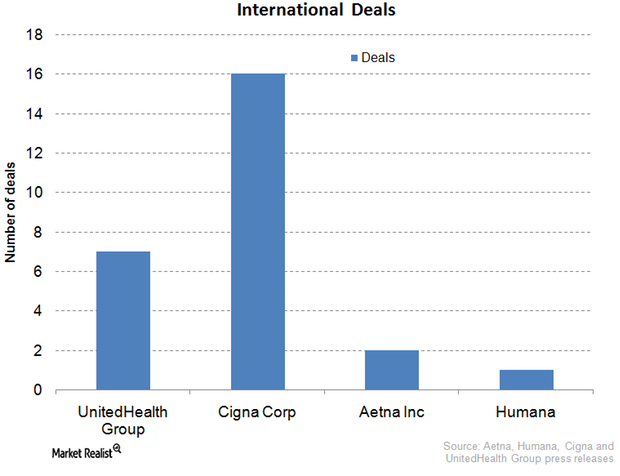
Cigna: International Expansion Key to Growth Strategy
International expansion is a hallmark of Cigna’s business. Cigna has inked deals in Turkey, Belgium, Brazil, Japan, Taiwan, Thailand, et cetera.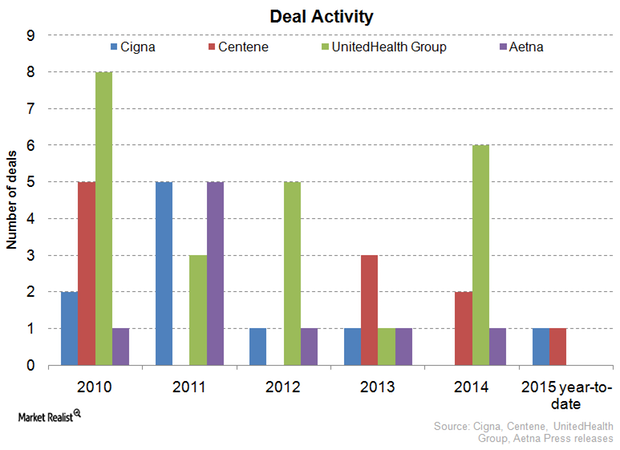
Cigna Diversifies Via Mergers and Acquisitions
Among Cigna’s major strategic mergers and acquisitions was HealthSpring, acquired in 2012 for a consideration of $3.8 billion.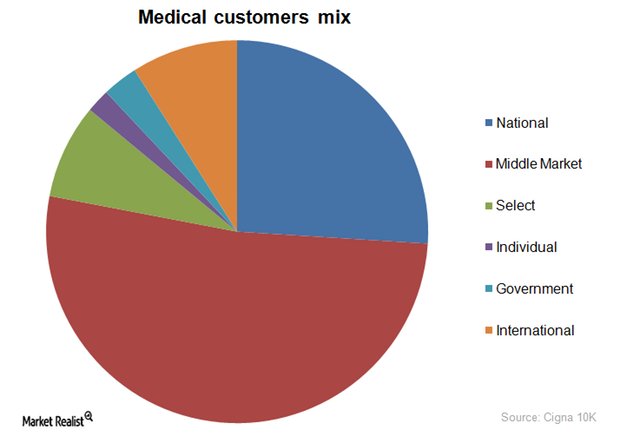
Cigna’s Customer Segments a Healthy Mix
Customer segments The players in the private health insurance industry (IYH) aim for a favorable enrollment mix to reduce taxes and other liabilities while at the same time generating sustainable profits. Accordingly, managed care organizations such as Humana (HUM), Aetna (AET), Anthem, Cigna (CI), and WellCare Health Plans (WCG) are increasingly focusing on government-sponsored and international enrollments to balance […]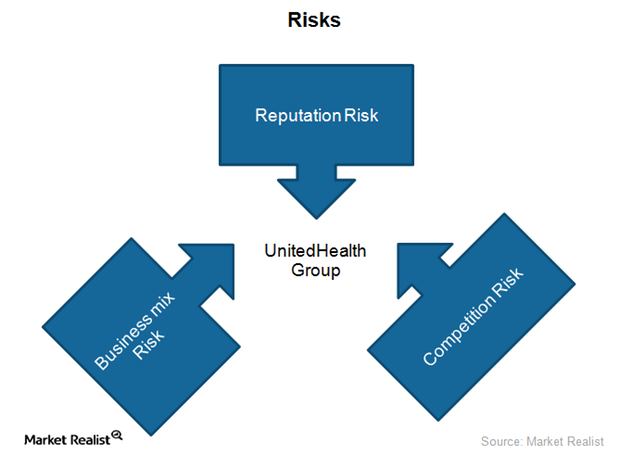
What key risks does UnitedHealth Group face?
UnitedHealth Group (UNH) is a health insurance provider. It faces a unique combination of business risks, including business mix and competition risks.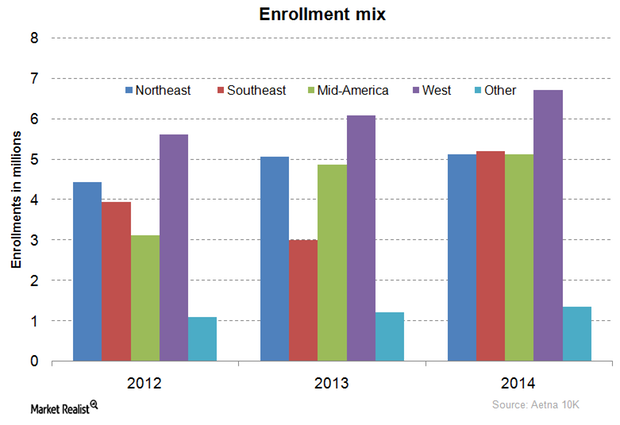
How Is Aetna’s Membership Distributed Across Its Key Markets?
Aetna’s membership is mainly concentrated in the western US, followed by the Southeast, the Northeast, the Mid-US, and finally consolidated international enrollments.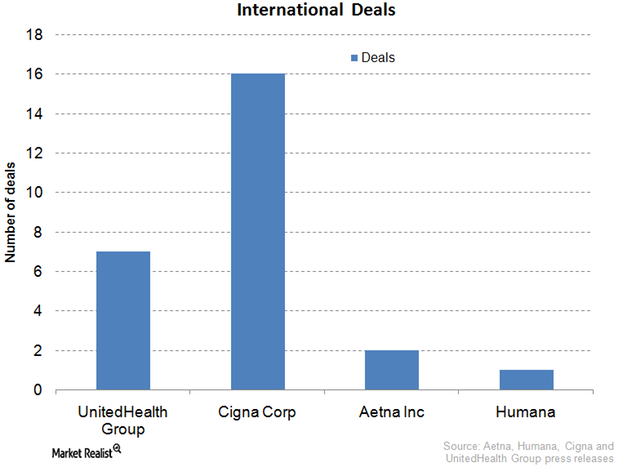
What’s UnitedHealth Group’s strategy for international expansion?
The private health insurance industry in the US has been expanding its footprint in international markets. International markets are less penetrated and competitive.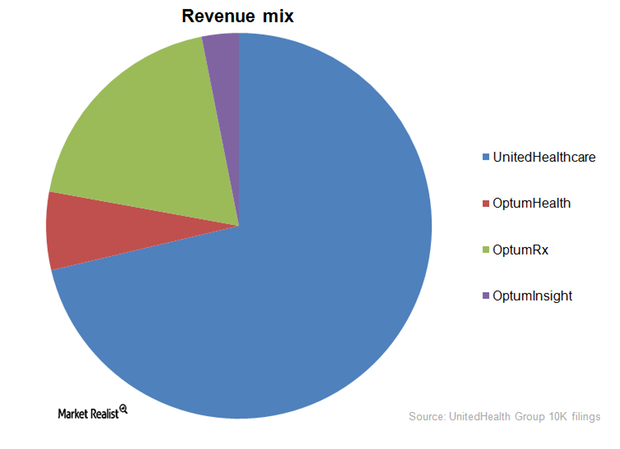
What are UnitedHealth Group’s key business segments?
Out of UnitedHealth Group’s (UNH) four business segments, UnitedHealthcare accounted for 71.3% of the company’s revenue.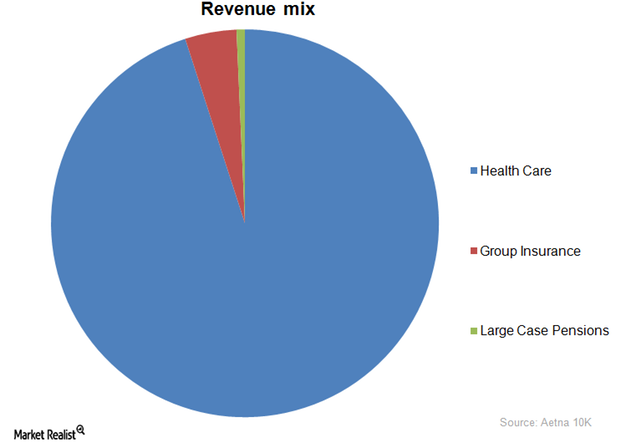
What Are Aetna’s Key Business Segments?
Out of Aetna’s (AET) three business segments, Health Care accounted for 95% of the company’s revenue.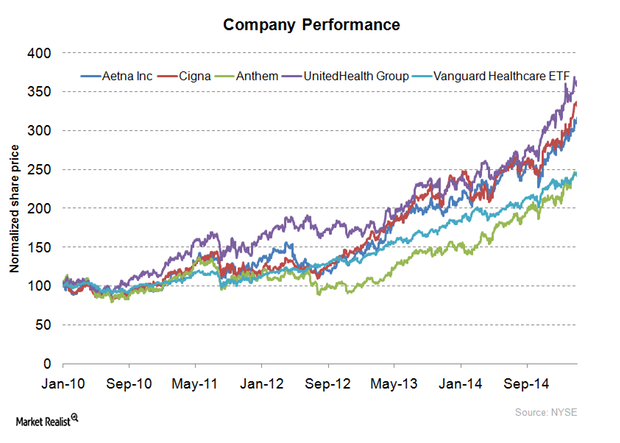
A Key Overview of Aetna, One of the Largest Insurance Providers
With a market capitalization of $35.1 billion, Aetna (AET) is one of the largest insurance providers in the US.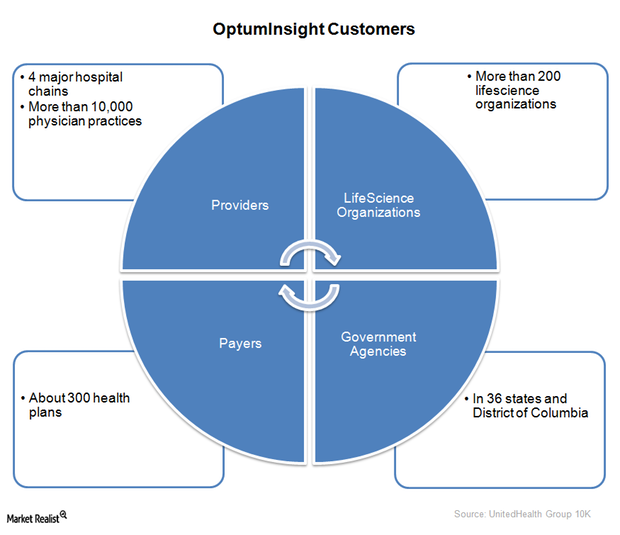
UnitedHealth Group’s OptumInsight – improving medical care
In 2014, OptumInsight released a population health analytics tool—OptumOne. It enables hospitals to improve the quality of care.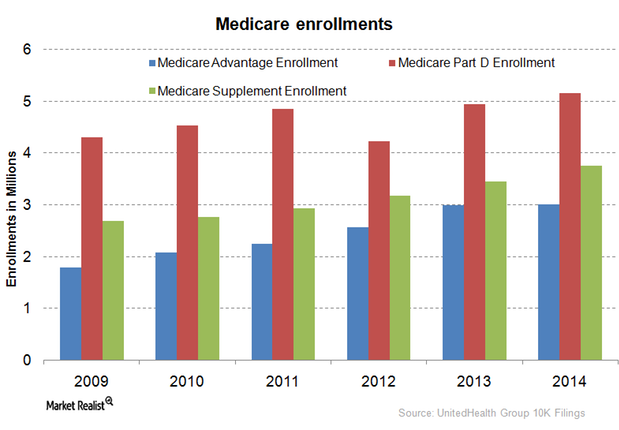
UnitedHealth Group provides services to Medicare beneficiaries
Medicare Part D is a federal government program. It subsidizes prescription drug expenses for Medicare beneficiaries.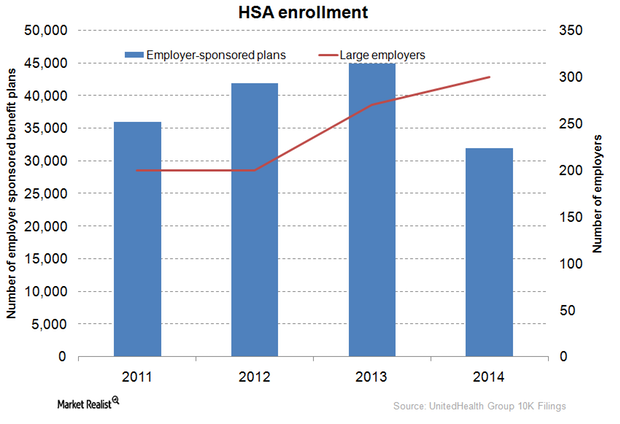
What are UnitedHealth Group’s consumer engagement products?
The private health insurance industry offers a diverse range of products. The products combine health plans with financial accounts to cater to different consumers’ needs.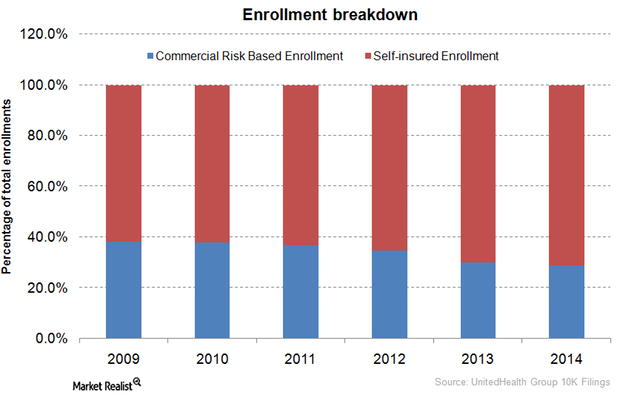
UnitedHealth Group’s employer-sponsored and individual insurance
Employer-sponsored coverage, a major form of insurance, increasingly adopted self-insured plans. They’re more cost-effective and flexible than fully-insured plans.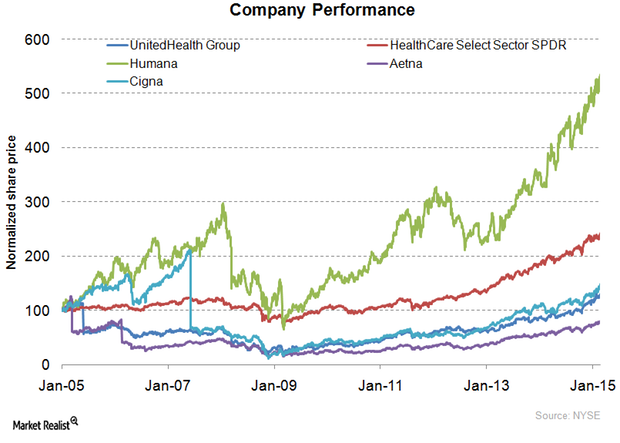
UnitedHealth Group: The history of a health insurance giant
With a market capitalization of $107.1 billion, UnitedHealth Group is the largest insurance provider in the US. It registered revenue worth $130.5 billion in 2014.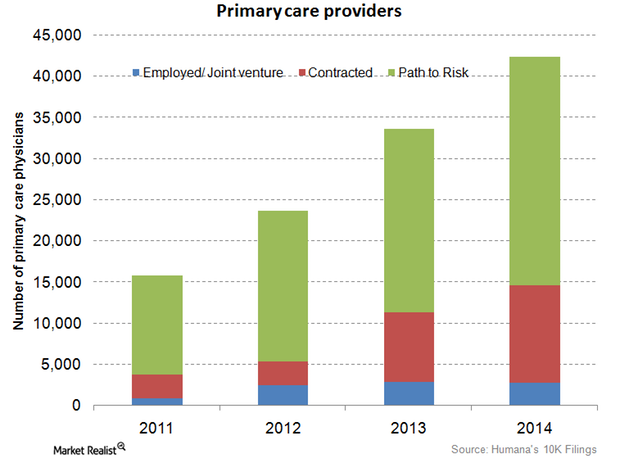
Humana employs and contracts more primary-care physicians in 4Q14
Humana’s employed and contracted primary-care physicians rose by 29.2% from 11,300 in 2013 to 14,600 in 2014.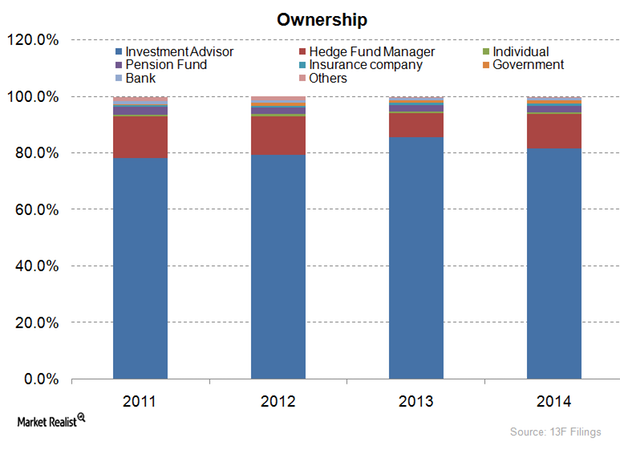
Most Humana stakeholders are mutual funds or advisers
Investment advisers or mutual funds are the main stakeholders in Humana, accounting for about 81.7% of its total ownership picture.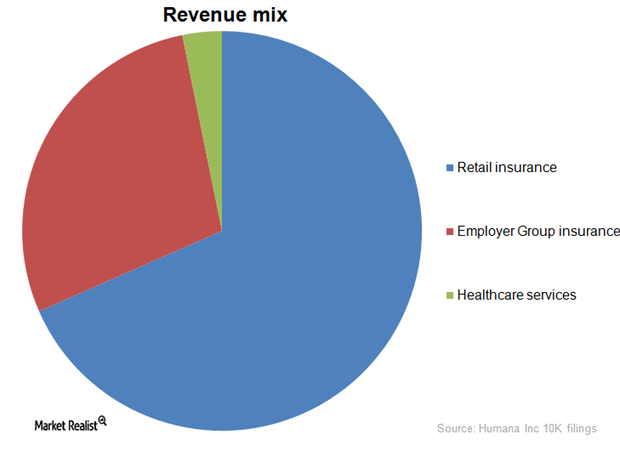
Humana’s Retail Insurance business segment is biggest earner
Humana’s retail insurance business segment contributes 66.5% of overall company revenues. Employer-sponsored programs follow with 27.6%.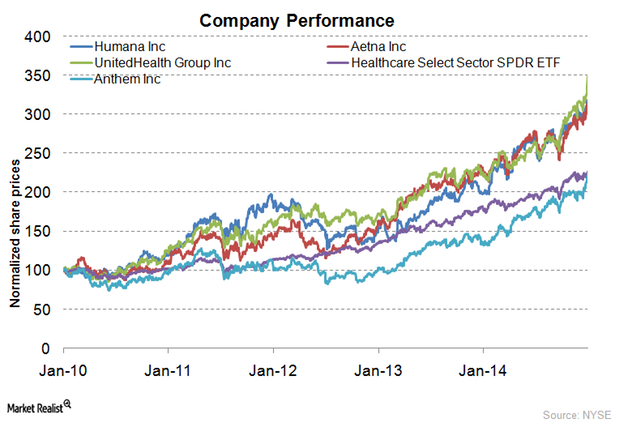
Humana: Unraveling the history of a health insurance giant
Humana (HUM) is the third-largest health insurance provider in the US, with over 13 million customers. Humana is also 73rd in Fortune 500 rankings.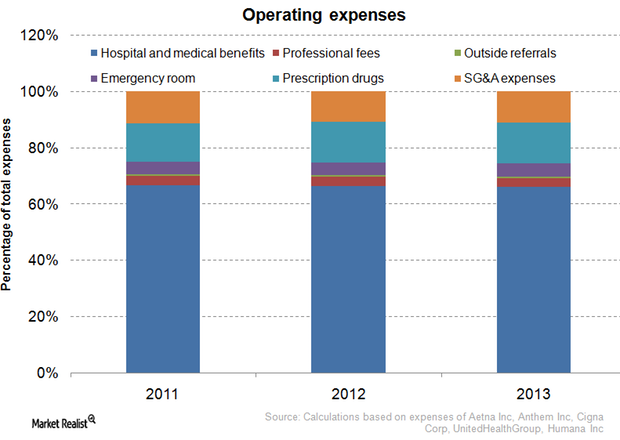
Understanding health insurance companies’ major operating expenses
The operating expenses of the private health insurance industry depend on the design of health plans and on the life history, age, and health of enrollees.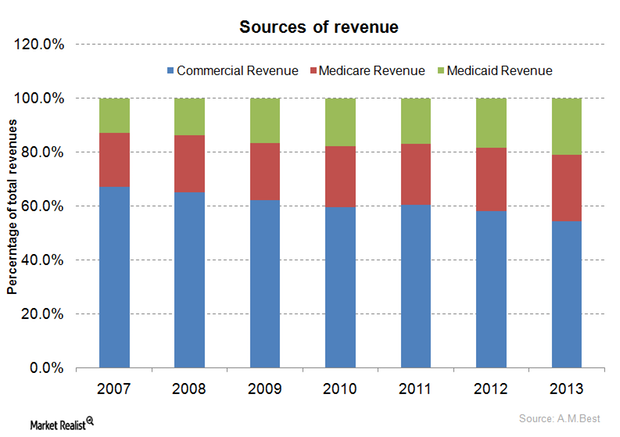
The health insurance industry’s major sources of revenue: A guide
The share of commercial revenues within the private health insurance industry’s total revenues decreased from 67.0% in 2007 to 54.3% in 2013.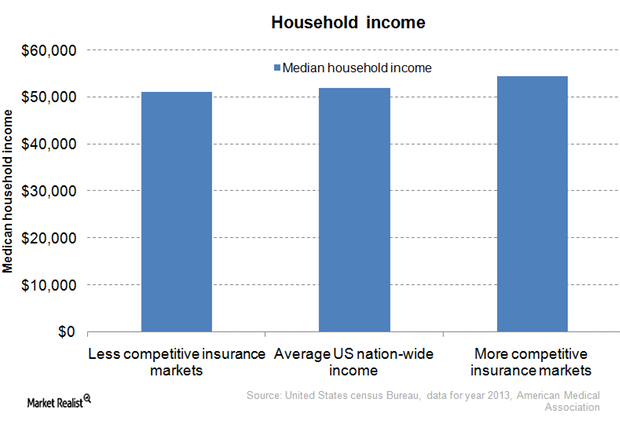
Health insurance monopolies: What you need to know
45 states have only two dominant health insurers accounting for half of the enrollments, giving rise to local market health insurance monopolies.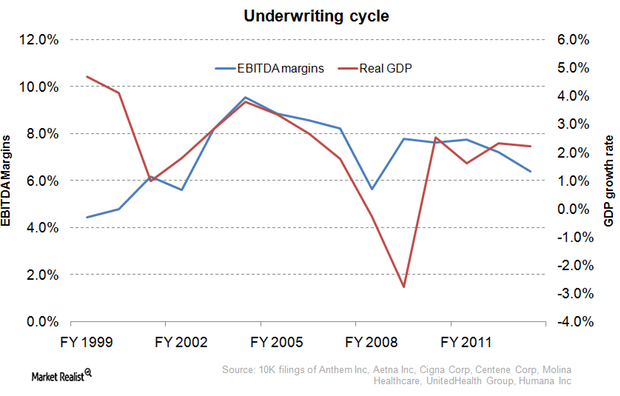
Underwriting cycle: What health insurance investors need to know
The underwriting cycle results from the uncertainty of predicting healthcare expenses and the fluctuating participants in the health insurance industry.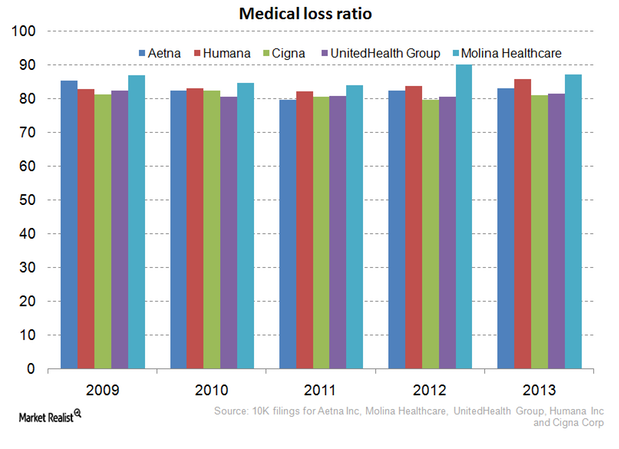
Why the Affordable Care Act hurts the managed care industry
The Affordable Care Act requires health insurers spend at least 80% of premiums on health expenses for small group plans and 85% for large group plans.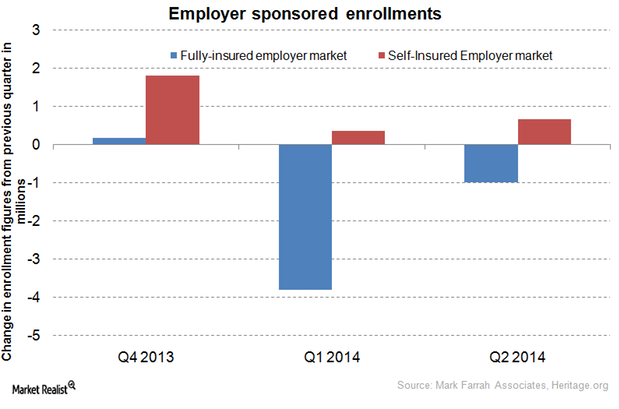
Shift to self-insurance plans affects health insurance stocks
As hospital utilization remains low, more employers are exploring the option of self-insurance to reduce their employee benefit costs.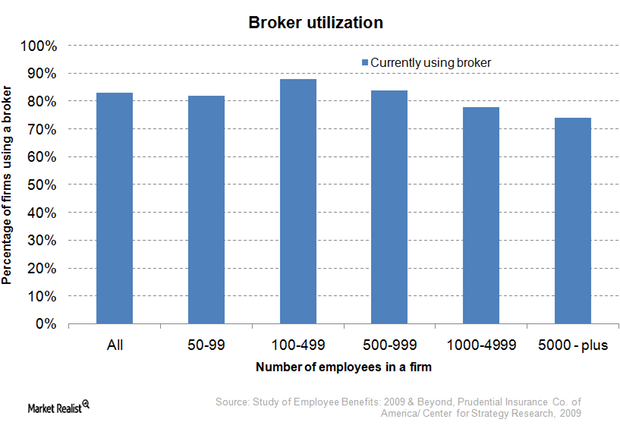
Must-know distribution channels for commercial health plans
The private health insurance industry categorizes commercial health plans as either individual plans, small group plans, or large group plans.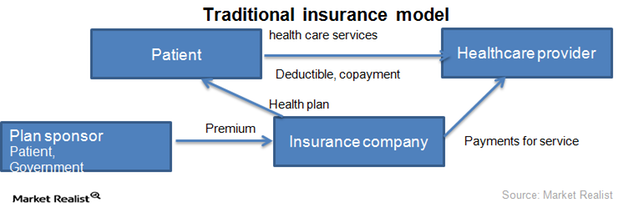
2 key business models of the health insurance industry
The health insurance industry runs on two business models: traditional insurance and managed care organizations.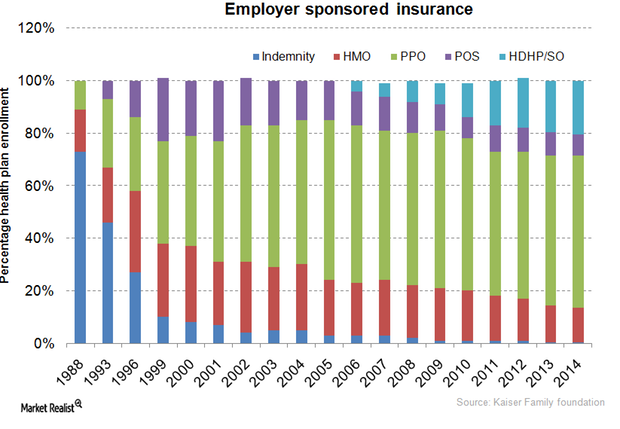
Your must-read guide to health insurance managed care plans
Employer-sponsored coverage is a key factor for nationwide enrollment trends of managed care plans and independent insurance plans.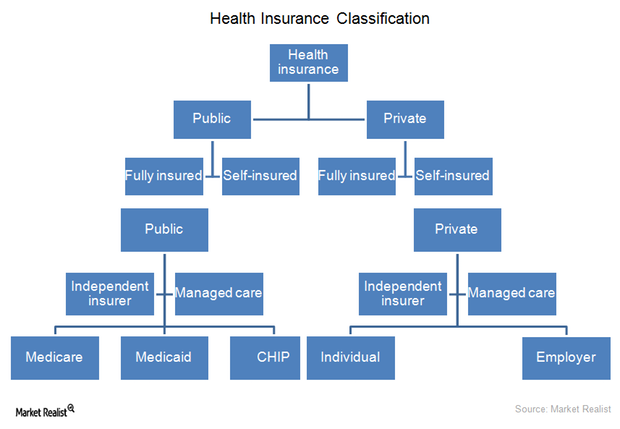
Making sense of health insurance types: An investor’s guide
The health insurance industry operates through two types of organizations: independent insurance companies and managed care organizations.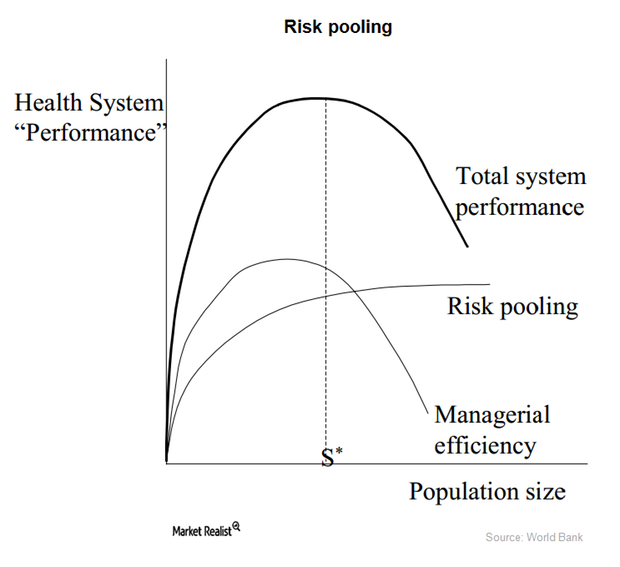
How the health insurance industry manages risks
The health insurance industry mainly gives individuals a risk management tool. People can’t predict the extent or timing of their their healthcare expenses.
